When you purchase through contact on our web site , we may take in an affiliate commission . Here ’s how it work .
An HIV diagnosis has n’t been a destruction sentence for geezerhood , thanks to knock-down medications .
Despite incredible progress , however , HIV(human immunodeficiency virus ) remain a spheric public wellness scourge , with 1.3 million Modern infections and around half that many deaths in 2022 alone .
Countries have teamed up through a United Nations program to end the AIDS epidemic by 2030. Can it be done?
While new HIV infection have dropped steady since theirpeak in 1995 , as citizenry live longer with the disease , the pool of people who are HIV - cocksure has only raise . People with HIV must consistently take medications to prevent the computer virus from becoming transmissible again or progressing to AIDS ( acquired immunodeficiency syndrome ) . As a resultant role , Modern infections could actually rebound fast if the earth does n’t dramatically ramp up the number of people being regularly treated , test and protected from novel HIV infections .
But we could point off that ricochet risk of exposure by the conclusion of the decade , expert say .
area around the existence havesigned onto an ambitious United Nations programwith a end to " subjugate the rate of new HIV infections and AIDS - related deaths to below the generative pace of 1 , " body politic by country , Quarraisha Abdool Karim , associate scientific director of the Centre for the AIDS Programme of Research in South Africa and a joint United Nations Programme on HIV / AIDS ( UNAIDS ) special embassador , tell Live Science . That would think each person live with HIV wouldinfect fewer than one extra personin their lifetime .

Medicines known as pre-exposure prophylaxis (PrEP) suppress the amount of HIV in a person’s blood until it’s undetectable.
If the curriculum is successful , we ’d see 200,000 new HIV infections and 130,000 AIDS - related destruction worldwide in 2030 — 90 % fewerthan in 2010 . While eradicating the computer virus would require a vaccine and cure , we could eventually drive HIV infections and death rate to near zero without those tools , Abdool Karim say .
" We do have the tools to stop AIDS as a public wellness threat . We do have the biomedical interventions , " she said . " The challenge is , how do weallget to that point in time ? "
relate : Could CRISPR bring around HIV someday ?
From the first treatment to ending AIDS
The first , imperfect HIV treatment , AZT ( azidothymidine ) , was approved in 1987 . Nearly four decades andmore than 40 millionAIDS - related destruction later on , we ’re still track down for a vaccinum and a cure for HIV , but our discourse have dramatically improved .
" We ’ve had really powerful treatments , really , since 1996 , but they just get better all the time,“Dr . Monica Gandhi , director of the University of California , San Francisco Center for AIDS Research and medical theater director of the HIV Clinic at San Francisco General Hospital , told Live Science .
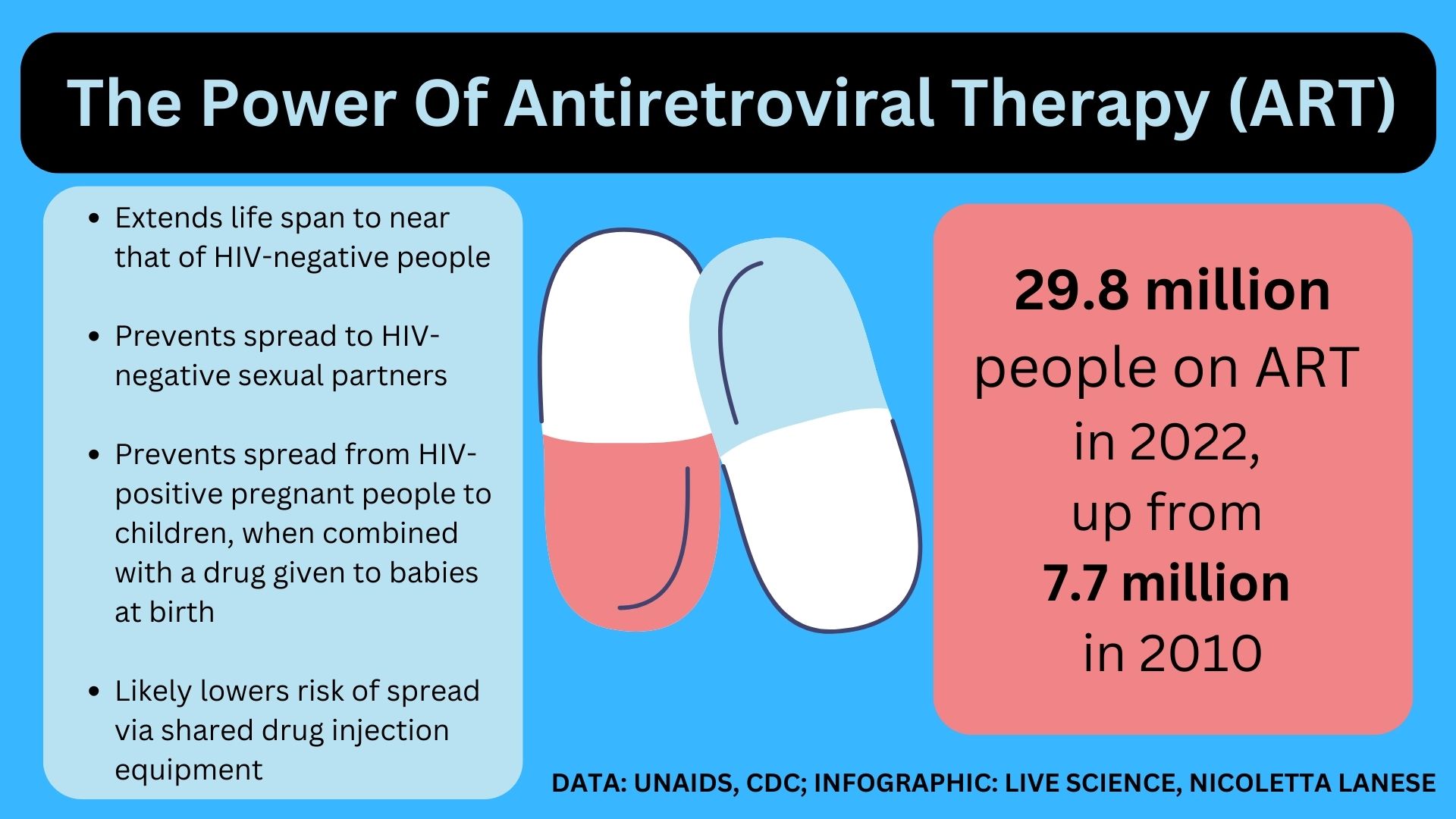
Today ’s standard treatment , compounding antiretroviral therapy(ART ) , uses several drugs to break up HIV ’s ability to replicate and invade immune cells . Given as daily contraceptive pill ormonthly or bimonthly injections , ART slashes the amount of HIV in a somebody ’s stock until it ’s undetectable . If asseverate , " viral suppression " stretch out a mortal ’s life span toabout that of HIV - negative peopleand extinguish their chance ofspreading HIV via sexuality .

Representatives of HIV organizations march along Whitehall in London, England on March 18, 2023, calling for an end to the stigma that still surrounds HIV.
" People living with HIV , on handling and undetectable , are not infectious — full plosive speech sound , end of statement — to their intimate partners,“Dr . Raphael Landovitz , Colorado - conductor of UCLA ’s Center for HIV Identification , Prevention , and Treatment Services , tell Live Science . Viral crushing also nearly wipe out HIV spreadto babies during pregnancy or childbirth , greatly cut spread via breastfeeding and likely lowers spread from share syringes .
We also have powerful medicines that forbid HIV - negative people from foreshorten the virus if exposed . know as pre - exposure prophylaxis ( PrEP ) , these drugs are available as casual pills . There ’s also an injectabledrug call cabotegravir(brand name Apretude ) that ’s collapse semimonthly . Some African countries have also licensed avaginal ring for HIV prevention ; it ’s less effective than PrEP anovulatory drug but works for a full calendar month . And safe use andvoluntary male circumcisionalso cut transmission system .
By 2014 , there was potent consensus that the drug we had could end the AIDS epidemic . But those drugs were n’t being rolled out fast enough to head off rebound in infection , UNAIDS monish . At that metre , models predictedthat if treatment and bar services did n’t reach more multitude over time , the number of multitude with HIV would billow to 41.5 million by 2030 . To forestall this , UNAIDS countersink forth challenging target to scale up the global HIV reaction . Hitting these targets would prevent 28 million unexampled HIV infections and at least 21 million AIDS - related death between 2015 and 2030 , they project .
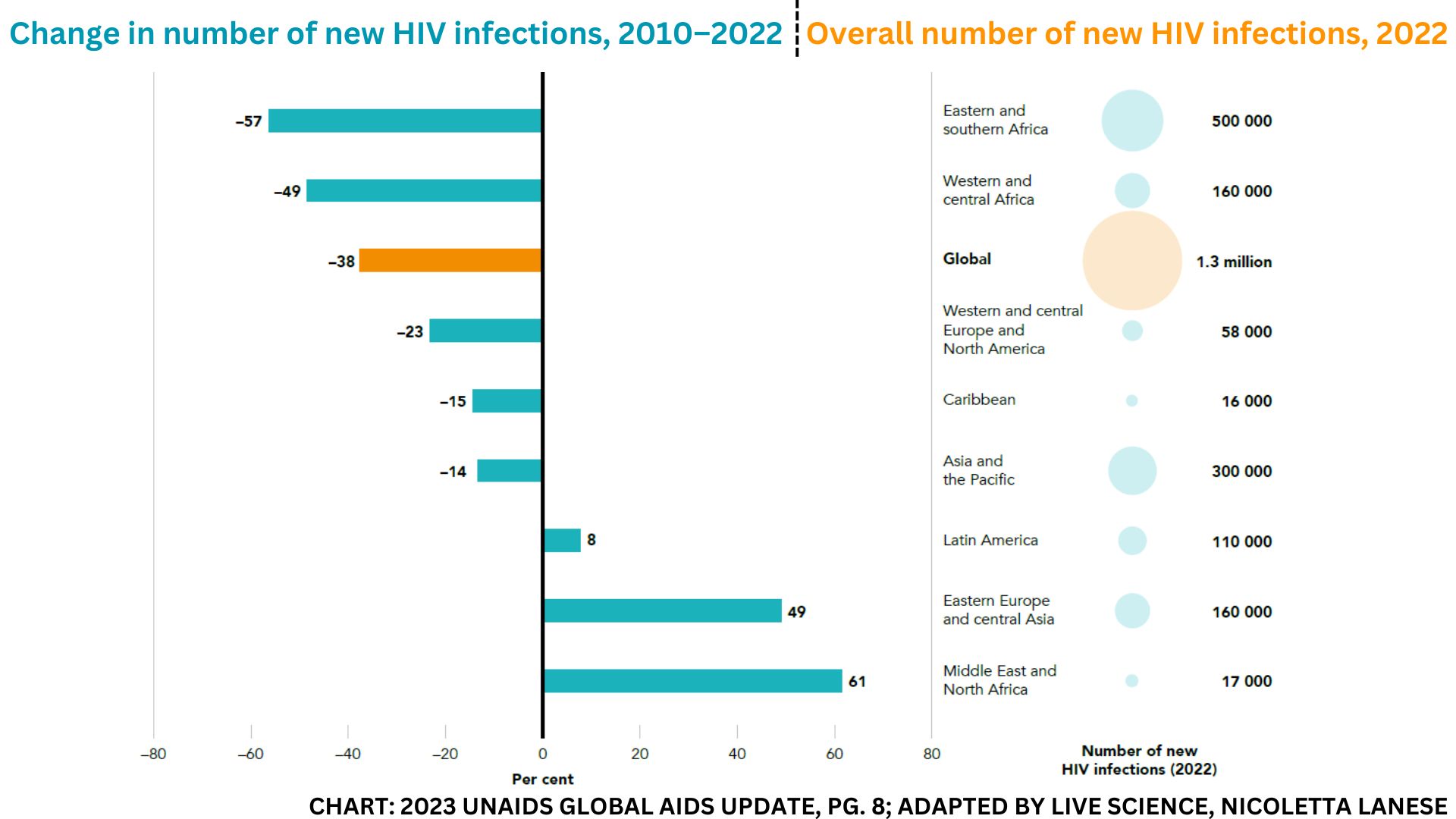
This chart appears in the"The path that ends AIDS: UNAIDS Global AIDS Update 2023."
One major destination , the " 95 - 95 - 95 " target , is prepare for 2025 . attain it would mean 95 % of people with HIV know their status , 95 % of those diagnosed take HIV drugs , and 95 % of those treated are " virally suppressed , " meaning the drugs keep them from spreading the infection via sex . This translate toaround 86 % of peoplewith HIV being virally suppressed .
Other 2025 targets shoot for to ensure that 95 % of the great unwashed at risk of HIV have access to prevention and that PrEP be made available to at least 10 million at - risk hoi polloi .
So far , we ’re not on target : In 2022 , only 76 % of the total 39 million hoi polloi with HIV worldwide were taking ART , and 71 % were virally suppressed , according tothe latest UNAIDS write up .

So what can we do to reach 95 % across the plank ?
Related : How are people cure of HIV ? Here ’s everything you need to bed
Vulnerable populations
A big hurdle to stop the AIDS epidemic is getting treatments to vulnerable populations , including children . In 2022 , only 57 % of the 1.5 million children under 15 with HIV received intervention , 46 % were virally crush and an gauge 84,000 died of AIDS - related illnesses .
That ’s partially because kids are n’t typically included in initial clinical trials for treatment , so there are comparatively few child - friendly formulas , Abdool Karim aver . The preferred intervention for shaver , a tablet that dissolves in water , was just approved in 2021 and has beenadopted only recently in many land . However , most other HIV drugs for kids smack bad , are difficult to swallow up or must be taken several times a day , UNAIDS take down , so improve these formulations could make their HIV regimens easier to maintain .
Long - playact ART options — meaning those that do n’t require everyday pills — are nonexistent for children under 12 , Gandhi said . To help oneself make long - act artistic creation worthy for new children , theNational Institutes of Health is supportingresearch into how to best adapt drugs O.K. for adults , she noted . But that deed over opens in 2024 , so it ’s unclear if it could make a ding before 2030 .
And even if well drug are widely available , " children are not going to be capable to get at antiretroviral therapy in a vacuum , " saidDr . Anjali Sharma , a prof of medicinal drug who now studies complication of HIV at the Albert Einstein College of Medicine in New York and has analyze ART adherence in different configurations .
" The paediatric upkeep really has to be integrated with other service , potentially the mom ’s intervention or things that are going to work with the fellowship as a unit , " she state .
have-to doe with : Kids under 5 with HIV are snuff it at high rates . Here ’s why .

The science is a first step , but access is what will render its true potential and note value .
strike the 95 - 95 - 95 target will also require better reaching teen young woman and vernal women , especially with bar and testing . Nearly 1 in 6 new HIV cases in 2022 were in miss and women ages 15 to 24 , many of whom are in sub - Saharan Africa .
Once diagnosed and started on ART , charwoman ’s viral curtailment rates are " high and so are survival benefits , " Abdool Karim said . Among all diagnosed women over 15,82 % had access to ARTand 76 % were virally oppress in 2022 . But starting ART first ask being test for HIV , and testing rates remain low in hard - hit regions , in particular among teens .
Many of the hardest - impinge on regions miss prevention programs for vernal women , and the few existing programme often miss young lady who are not in school . Girls face a deficiency of Education Department , poverty and food for thought insecurity have an particularly mellow endangerment of HIV , as do girls with older male partners . Intimate - partner violence and sexual coercion often imply they can not control when they are uncover to HIV . Plus , in some commonwealth , HIV services demand parental consent , which can also reduce girls ' access to bar and discourse .
Improving girl ' access to discreet prevention services as well as sex education — both in and out of school — will be key to scale down their HIV charge per unit . Cabotegravir , which is " stunningly effective against vaginal acquisition of HIV , " could be a powerful tool for HIV prevention in char , Landovitz said .
Other population that are far from the targets include transgendered multitude with HIV , an estimated 44 % of whom are on ART , and HIV - incontrovertible Isle of Man who have sex with Isle of Man , who have 78 % ART coverage . In accession , just 65 % of HIV - positive sex workers and 69 % of HIV - positively charged people who inject drugs take ART . Compared with the general adult population , these groups have far higher HIV prevalence , ranging from fourfold greater among sex worker to 14 - fold greater among transgender people .
And those numbers could be an undercount , as many land do n’t chase after these population . Punitive laws , constabulary harassment , abrasive mark and social tabu keep many people out of HIV care , while high rates of incarceration and sexual violence also arouse their risk of acquiring HIV . Lifting discriminatory policy and wander HIV care into trusted , community - base program will be key to hand these demographics .
relate : Patient ’s resistant system ' naturally ' cures HIV in the 2d case of its kind
Cost barriers
The tools to terminate the epidemic by 2030 will bring , but only if they get to the people who require them . " The science is a first step , but admittance is what will translate its honest potential and economic value , " Abdool Karim told Live Science .
For instance , the number of citizenry taking PrEP pill rise up more than tenfold from 2019 to 2022 . But cabotegravir , a potential plot record changer , is not yet wide used due to its high cost — $ 3,700 per dosein the U.S. The drug ’s non-profit-making damage will be around $ 30 a battery-acid , the drug ’s makerrecently distinguish the South African news program outlet Bhekisisa , and generic reading will bemanufactured in approaching years . But the current high price means HIV programs have yet to fold cabotegravir into their budgets , Landovitz said .
" There ’s still not a fall of cabotegravir to be had anywhere in Africa , " where some of the highest rates of new HIV transmission occur , Abdool Karim state .

And regardless of the type of ART they take , a patientshould have their viral load checked regularly . In 2022 , 21 million multitude underwent routine viral - load testing , up from 6 million in 2015 . Viral - lading tests are expensive , though , so proxy measure — such as a piddle testGandhi and colleagues plan to get over ART levels — could avail fulfil the same purpose cheaply .
In addition , an estimated 25 % of people stop ART intervention , sometimes for six month or more , often because they face brand , ca n’t get to the clinic or ca n’t give treatment . These individuals , many of whom come from vulnerable population , represent a grow proportion of the AIDS cases interpret in hospitals .
" That is preventable and avoidable and really typify a failure on many floor , " Sharma told Live Science . " But the bankruptcy is n’t really the drug itself . " It ’s a bankruptcy of the support organisation that could keep people on ART , she said .

Related : HIV may hide out in brain cubicle , ready to infect other organs
Success stories and further work
Despite the hurdles , some country are well on their way to meet UNAIDS ' destination . Botswana , Eswatini , Rwanda , the United Republic of Tanzania and Zimbabwe have already dispatch the 95 - 95 - 95 target rig for 2025 , and an additional 16 body politic are tightlipped to extend to these milepost .
The U.S. trail behind . In 2021,75 % of the the great unwashed diagnosedin the country received " some HIV care , " and 66 % were virally inhibit . piece who have sex with men made up the mellow proportion of fresh infections in the U.S. , withBlack , Hispanic and Latino populationspredominantly affected .
Countries that have hit the 95 - 95 - 95 prey extend universal , free nontextual matter access , Landovitz take note , while the U.S. governance only hasprograms to aid cover uninsured people ’s HIV treatment . racialism , homophobia and transphobia often keep people from getting upkeep , he said . And peculiarly in urban centers , people share with housing insecurity , centre use and mental health issuesstruggle to get at ART consistently , Gandhi said .
Eastern Europe and Central Asia also lag far behind , with just 51 % of people with HIV getting artistic production and less than half being virally suppressed .
Related : Oldest ' nearly staring ' HIV genome found in forgotten tissue sample from 1966
Beyond 2030
We face up many obstacles on the route to cease the AIDS epidemic — but we do hold all of the tools to get there , Abdool Karim , Sharma , Gandhi and Landovitz agreed . By using those putz effectively , we could begin to meaningfully repel the number of Modern HIV infection toward zero . At that point , HIV would become a manageable , continuing disease of the elderly .
— field hints at how ' elect accountant ' stifle HIV
— HIV vaccine stimulates ' rarified resistant cell ' in former human trial
— Scientists zoom in on HIV inside a test thermionic vacuum tube , find critical steps in infection
Already , about a quarter of people with HIV worldwide , and about one-half of adult with HIV in Western and Central Europe and North America , are at least 50 years old . " They ’re grow previous with HIV ; they ’re not exit from HIV or AIDS , " said Sharma , whose research focuses on aging population with HIV .
But that does n’t mean the pursuance for an HIV vaccine or therapeutic is any less of import , even if neither is likely to materialise in the next seven year , Abdool Karim said .
" We need to continue our investments to find a vaccine , to see a therapeutic , " she told Live Science . " Because that will then say , ' That ’s it . ' "