When you buy through links on our site , we may earn an affiliate perpetration . Here ’s how it work .
woman’s doctor should be inform of the signs of rarefied , " flesh - eating " infection , physician monish , because these dangerous infection can sometimes infiltrate the vulva .
In a young case report published April 8 in the journalBMJ Case Reports , U.K. physician describe three patients who were found to havenecrotizing fasciitisof the vulva . The vulva let in the external distaff genitalia , such as the labia majora and labia minora , for lesson .

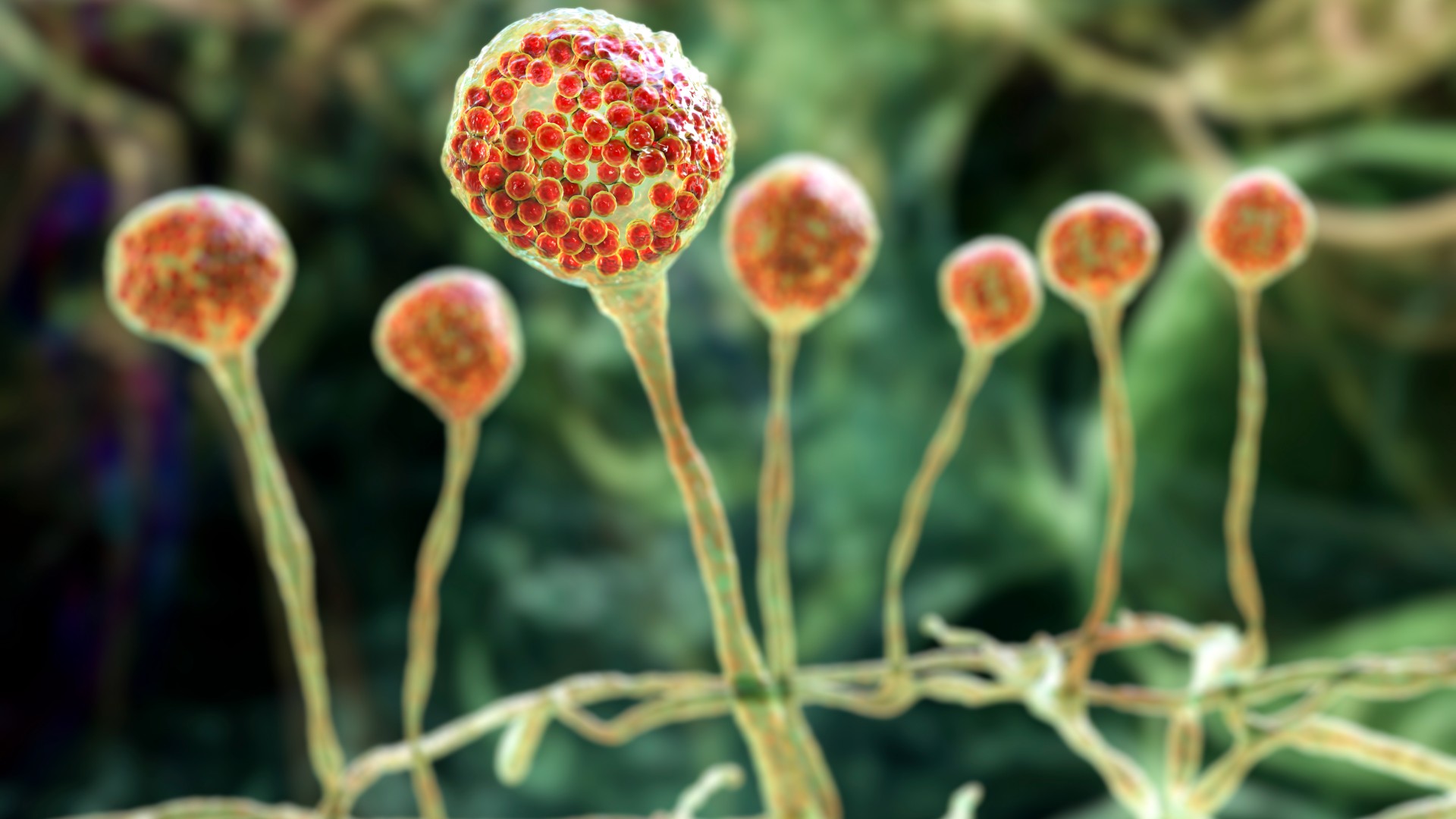
Necrotizing fasciitis is a dangerous bacterial infection that quickly kills soft tissues of the body. A new series of case reports highlights how the infection can affect the external female genitalia.
" Necrotizing fasciitis ( NF ) , also known as flesh - consume disease , can rise up when sure bacterium enter the skin through a combat injury — a cut , abrasion , burn , operative wound , or even an worm bite,“Bill Sullivan , a professor of microbiology and immunology at Indiana University , who was not involved in the case composition , told Live Science in an email . " NF can occur anywhere skin or tissue is breached , include genitalia . "
In necrotizing fasciitis , bacteria infiltrate the fascia , which is the connective tissue surrounding brawniness , nerves , fat and pedigree vessels . The infection apace do soft tissues to die , or " necrotize , " and spreads through the body very quickly .
Related : scientist are build an ultimate atlas of the vagina . Here ’s why .

The fount report authors , who are affiliated with the Shrewsbury and Telford Hospital in England , partake in these three case to notify other gynaecologists of the hypothesis of vulvar affaire in necrotizing fasciitis cases .
They take down that their infirmary has assure a meaning uptick in chassis - eat infections in recent days , with 20 shell consider between 2022 and 2024 when only 18 had been report in the preceding decennary . In addition , several EU statesandthe U.S.have describe increases in invasive grouping A streptococcus , an infection that can lead to necrotizing fasciitis .
If the infection is becoming more common , doctors should experience the grandness of rapid treatment , the display case report author accentuate .
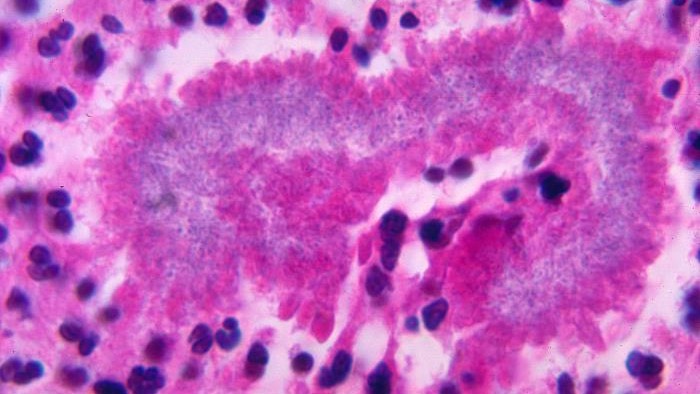
" It ’s an passing fast-growing infection that can gain to a animation - threatening situation in 24 - 48 hours , " Sullivan said . " After these bacteria get into the skin , they release potent toxins that direct to speedy tissue destruction , liquefying muscle , nerves , and lineage vessels . "
The subsequent loss of blood supply to the affected soundbox part makes treating necrotizing fasciitis with antibiotics difficult , Sullivan explained ; infected field sometimes need to be surgically cut out of the eubstance . to boot , once the bacteria get into the blood stream , they can causesepsis , a dangerous , dead body - wide-eyed immune reaction , potentially extend to organ unsuccessful person and death .
In the display case report , the Doctor of the Church distinguish the eccentric of two patient role who come to the emergency room with necrotising fasciitis of the vulva , as well as a third who developed the infection following a postoperative wound .

The first patient role was alerted to the infection when she found a small smear on her Mon pubic bone — the fatty tissue paper over the pubic bone . She ab initio went to her master care doc , who prescribed antibiotic drug . However , the spot worsened over the next five twenty-four hours , which lead in necrotizing fasciitis that spread to her labia majora , left hip and lower abdomen .
At the ER , the septic tissue paper was surgically get rid of , or " debrided . " But " despite intensive maintenance whole ( ICU ) management for systemic infection , " the patient die of sepsis only 28 hour after diagnosis .
The second affected role came to the ER with a one - week chronicle of get a lump on her labia majora , which bend out to be an infected abscess . Over the next 12 hours , the upper third of her labia majora break down from necrotizing fasciitis . The affected role at long last needed three debridements to control the contagion , after which she undergo rehabilitative operating theater for the baffled tissue . " The wound has since healed well , " her doctor noted .
The third patient suffered necrotizing fasciitis after a surgical wound got infected ; she had gotten a hysterectomy as a treatment for fibroid . This patient ultimately survived after having the infected tissue surgically removed and being given encompassing - spectrum antibiotics .
" NF is very rarified , " and it most often arises in people with conditions that weaken the immune organization , such as diabetes or cancer , Sullivan explained . An estimated700 to 1,200 casesare seen in the U.S. each yr . About 500 cases are reported annually in the U.K. , or about 0.4 to 0.53 cases per 100,000 people , the case theme authors note .
Vaginal necrotizing fasciitis is even more rare , as masses are more likely to have skin injury on more let out part of the dead body .

" Vaginal NF could be contracted through scratchy sex , a piercing , or decorative and operative procedures , " Sullivan say . " The deathrate charge per unit of vaginal NF isestimated to be up to 50 % . "
— Scientists invent 1st ' vagina - on - a - chip '
— Controversial ' vaginal seeding ' shows promise in pocket-sized trial , but questions remain

— musculus - bring around gelatin could be a ' new frontier ' for cover pelvic floor legal injury , very early study suggests
The case report author press other gynecologists to keep an heart out for any sign of an contagion that could grow into necrotizing fasciitis , and they also emphasized that " time is of the essence " when treating the status .
" Vaginal NF could be consider more dangerous in the sense that it might be more unmanageable to diagnose in time , " Sullivan say . " Gynecologists may not have NF on their symptomatic radar , and surgical interposition , which are usually want to block NF from broadcast and hit beat tissue paper , may be limited . "

Recognizing the disease quickly is key to saving patients ' lives . " Delayed diagnosis can lead to delayed treatment , increase the betting odds of sepsis and death , " Sullivan say .
This article is for informational purposes only and is not meant to offer medical advice .
You must confirm your public display name before commenting
Please logout and then login again , you will then be actuate to enter your presentation name .